B e f o r e :
MR JUSTICE FOSKETT
____________________
Between:
| |
XXX
|
Claimants
|
| |
- and
|
|
| |
KING'S COLLEGE HOSPITAL NHS FOUNDATION TRUST
|
Defendant
|
____________________
Elizabeth-Anne Gumbel QC and Mr Richard Cartwright (instructed by Irwin Mitchell LLP) for the Claimants
John Whitting QC (instructed by Kennedys Law LLP) for the Defendant
Hearing dates: 21, 22, 23 and 27 February 2018
____________________
HTML VERSION OF JUDGMENT APPROVED�
____________________
Crown Copyright ©
Mr Justice Foskett:
Introduction
- At the outset of the trial I made an anonymity order. Although, as will appear, the case is a "wrongful birth" claim and the Claimants are adults who are not "protected parties", the substance of the case relates primarily to the needs of a seriously disadvantaged 7-year old boy and it seems to me to be an appropriate case for such an order. Such an order is always subject to review, but it seems to me to be a justified order in this case at the moment.
- The boy, who will be referred to as 'XXX' in this judgment, was born at the Princess Royal University Hospital in Orpington, Kent, on 22 November 2011. The Defendant Trust is responsible for the hospital.
- After XXX was born it was discovered that he possessed a chromosomal abnormality called a '22q11.2 deletion' (otherwise known as DiGeorge syndrome). Although the case is not at this stage concerned with the nature of his disabilities, it is alleged on his behalf that he has suffered and will continue to suffer developmental delay and learning disability, with intellectual abilities far lower than would otherwise have been expected, and will require "further multiple heart surgeries" in the future. He has already undergone two surgical corrections to the heart defect referred to below (see paragraphs 19-23 below) and he remains under the supervision of the cardiac unit at Evelina London Children's Hospital. There is a question (that cannot yet be answered) about his ability to live independently in the future.
- Had his mother had an amniocentesis, the chromosomal abnormality would have been revealed. It is accepted that she would have received advice about the consequences of the abnormality and that it would have been at a time when the possibility of a termination of pregnancy would have been offered. Her case is that she would have opted for a termination.
- She underwent a routine 20-week ultrasound fetal anomaly scan at the hospital on 7 July 2011. It was carried out by Mr. Don Jayasinghe, an experienced sonographer. It is common ground that the fetus at that stage would have possessed an abnormal heart structure that, if identified, would have led to a fetal echocardiogram and an offer of an amniocentesis.
- The primary issue in the case is whether Mr Jayasinghe, who essentially reported that the scan was normal, negligently missed the abnormality that existed and thus failed to refer XXX's mother on for further investigation. There is a secondary issue, namely, whether, as she alleges, XXX's mother would have opted for a termination when told of the potential consequences of the chromosomal abnormality.
- The issues are narrow. Each side contends that the answer to the first issue is simple. It can be stated simply, but it is less easy to resolve given the debate between the expert witnesses. A list of the expert witnesses called on each side appears in Appendix 1 to this judgment.
- However, it is right to observe that when certain infelicities and ambiguities of expression in the various expert opinions about the appropriate scanning techniques were analysed, the picture became clearer. The concepts are a little difficult for a layman to understand and it is not made easier when different expressions appear to be used for the same thing. However, one advantage of oral evidence in a case such as this is that these difficulties become less once the uncertainties of the language are exposed and explained. One regrettable feature of this process in this case, in my view, is that it took until at least the conclusion of all the oral evidence before the picture became clearer.
- The difficulty remains, however, in conveying accurately and comprehensibly to a lay reader of a judgment such as this precisely what is meant by a particular aspect of the scanning technique. As most people will know, the technique itself involves a dynamic process of moving a transducer over the mother's abdomen in search of certain important features of the fetal anatomy in a fetus that may itself be moving. Ms Hazel Edwards, the expert sonographer who gave evidence on behalf of the Defendant, said that it is "hard to verbalise an ultrasound scan". I think that sums up the difficulty accurately.
- I will return to these issues where relevant in due course.
The legal test
- There is no dispute about the legal framework for the decision. Mr Jayasinghe's actions have to be judged by determining whether he acted with reasonable care according to the standards of the reasonably competent and well-informed sonographer on the basis of what contemporary standards required in July 2011. Ms Elizabeth-Anne Gumbel QC, for the Claimant, referred me to Penney v East Kent Health Authority [2000] Lloyd's Rep Med 41, where issues of a comparable nature were considered.
- In this connection Mr John Whitting QC, for the Defendant, referred me to Lillywhite v University College London Hospitals NHS Trust [2005] EWCA Civ 1466. His contention, based upon the approach adopted by the majority of the Court of Appeal in that case, is that where, as he suggests is the case here, a claimant cannot positively identify the scanning mistake which had been made (other than the fact that the abnormality had actually been missed), the defendant would escape liability if it could demonstrate positively a reasonable and plausible explanation for missing it. I will return to that contention if it arises.
The nature of the fetal anomaly scan
The normal fetal cardiac anatomy
- Before understanding the nature of the anomaly that is said on behalf of the Claimants to have been negligently missed, it is important to understand the normal fetal cardiac anatomy.
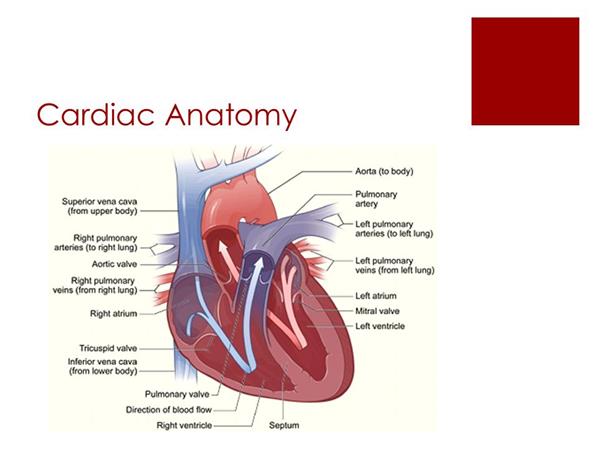
- Mr Whitting helpfully produced a diagrammatic representation of the normal heart as an Appendix to his Opening Note. I reproduce that diagram in Appendix 2 to this judgment. It helps to understand the relative locations of the individual features of the heart.
- In the normal cardiac anatomy, the aorta leaves the left ventricle and the main pulmonary artery leaves the right ventricle. The aorta and the main pulmonary artery are two of the "great vessels" of the heart. The left ventricle is the main pumping chamber of the heart, the function of which is to pump oxygenated blood through the aortic valve into the aortic arch and thence to the rest of the body. Deoxygenated blood returns to the heart through the veins and via the right atrium through the tricuspid valve into the right ventricle. That ventricle pumps the blood through the pulmonary valve and through the pulmonary artery to the lungs where the blood is re-oxygenated.
- In the normal heart, there should be an intact interventricular septum (the 'septum' illustrated in the diagram in Appendix 2) and a left and right ventricular outlet ('LVOT' and 'RVOT' respectively) which cross over each other, broadly at right angles (often referred to as the "offset cross"). The LVOT is the aortic outflow tract and the RVOT is the pulmonary artery outflow tract. The reason for the cross-over is that each goes in a different direction: the aorta goes in the direction of the right shoulder and the main pulmonary artery goes in the direction of the spine. Although the diagram in Appendix 2 is inevitably two-dimensional, a sense that these two vessels go in different directions can be obtained from it.
- The developing heart of a fetus at 20 weeks is, of course, very small. Dr Patricia Chudleigh, the expert sonographer called for the Claimants, described the heart at this stage as being "the size of an olive" and the working assumption is that it occupies about one-third of the chest cavity of the fetus at that stage of development.
- Notwithstanding its small size, its essential features can or should be capable of being visualised on a properly conducted ultrasound scan, as indeed should any defects in its structure (subject to the issue of "mimicking" to which I will refer in due course and to the issue of whether some defects may be missed despite using ordinary care and skill: see paragraphs 22 and 79-104 below).
The anomaly in XXX's case
- The cardiac defects demonstrated in XXX's case were in the form of a truncus arteriosus (otherwise called a common arterial trunk 'CAT') and a large ventricular septal defect ('VSD').
- The form of truncus arteriosus in this case meant that only one vessel left the ventricles, the effect being that both oxygenated and deoxygenated blood mixed in the single trunk that rose from both ventricles. This occurred because of an incomplete separation of the aorta and pulmonary artery in embryonic life, a separation that ordinarily takes place. The consensus amongst the experts appears to be that there was no LVOT and no RVOT, merely one ventricular outlet. (An alternative way of describing the defect is that the single ventricular tract was both an LVOT and an RVOT. The consequence is the same.) However, another way of describing the position, as I understood the evidence, was that there was an RVOT, but no LVOT (which is the way Dr Bu'Lock and Mr Howe eventually described the position). At the end of the day, I do not think a conclusion as to which of these various descriptions more accurate is important to the outcome of the case save to the extent that the particular physiological cardiac configuration in XXX's case is of relevance to what would have been seen on the scanning: the important factor for present purposes is that there was only one ventricular outlet. I will return later to the issue of the effect that the particular physiological cardiac configuration in XXX's case may have had on the scanning undertaken (see paragraphs 79-104 below). However, the net physical effect of the anomaly is that XXX became desaturated (in other words, his oxygen saturation levels were reduced) leading to potentially very severe problems.
- Whilst it is common ground that it is not incumbent on a sonographer to make a diagnosis as such of any form of truncus arteriosus (that would be for the fetal cardiologist after referral and an echocardiogram), any inability to identify on ultrasound examination an LVOT and an RVOT would require referral for further investigation because it would be suggestive of an anomaly.
- Given the nature of the anomaly in this case, variously described as above, it is obvious that it would be impossible for a sonographer to visualise both a real LVOT and a real RVOT: the sonographer would only be able to visualise one real outlet tract, but it would be neither a real LVOT nor a real RVOT (unless it is correct to say that there was a real RVOT in this case in which case a real RVOT would have been seen, but no real LVOT could have been seen). If a sonographer, faced unknowingly with such an anomaly, records that he or she did visualise two separate outlet tracts, one left and one right, then he or she must have been seeing some anatomical feature that mimicked the ultrasound view of these tracts. This is where the concept of "mimicking" comes into play.
- Again, I will return to that particular issue in due course because the case now advanced for the Defendant is that a very unusual feature of XXX's cardiac anatomy made it possible for Mr Jayasinghe to believe that he saw both a normal LVOT and a normal RVOT whereas, in fact, he could not have done so (see paragraphs 79-104 below) and that this occurred whilst he was carrying out an accepted, and thus reasonable, scanning technique.
The prevailing standards in 2011
- It is common ground that the scanning technique adopted by Mr Jayasinghe falls to be assessed by reference to the standards of the time when the scan was carried out in July 2011. However, it is important to see how the relevant technique developed and the reasons for the development.
- The International Society of Ultrasound in Obstetrics and Gynaecology ('ISUOG') is, as its name suggests, an international organisation that offers guidance and training to its members. In a guideline first issued in December 2005 (recognised by the parties to be non-mandatory) entitled 'Cardiac screening examination of the fetus: guidelines for performing the 'basic' and 'extended basic' cardiac scan', ISUOG reviewed briefly the history in this way:
"Congenital heart disease (CHD) is a leading cause of infant mortality, with an estimated incidence of about 413 per 1000 live births. Between 1950 and 1994, 42% of infant deaths reported to the World Health Organization were attributable to cardiac defects. Structural cardiac anomalies were also among the most frequently missed abnormalities by prenatal ultrasonography. Prenatal detection of CHD may improve the pregnancy outcome of fetuses with specific types of cardiac lesions."
- The guideline referred to the 'basic' and 'extended basic' cardiac ultrasound examinations, the former relying on what is called a "four-chamber view" of the fetal heart. It involves (or should involve) more than simply a count of the number of chambers and requires an analysis of certain physiological features and an observation of the cardiac rate and rhythm. Nothing turns on that in this case. Mr Jayasinghe obtained (and indeed recorded) a satisfactory four-chamber view (see paragraph 52 below).
- The guideline goes on to describe what is said to be an 'Extended Basic Cardiac Examination' which is said to be as follows:
"If technically feasible, routine views of the outflow tracts should be attempted as part of an 'extended basic' cardiac screening examination. Evaluation of outflow tracts can increase the detection rates for major cardiac malformations above those achievable by the four-chamber view alone. Additional views to the basic cardiac examination are more likely to identify conotruncal anomalies such as tetralogy of Fallot, transposition of the great arteries, double outlet right ventricle, and truncus arteriosus.
An extended basic examination minimally requires that normal great vessels are approximately equal in size and that they cross each other at right angles from their origins as they exit from their respective ventricular chambers. Failure to confirm these findings in a well-visualized study warrants further evaluation." (Emphasis added.)
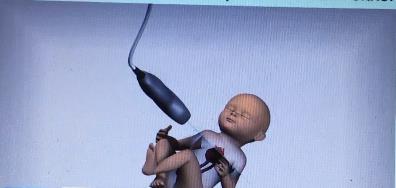
- The guideline goes on to describe the scanning technique required to achieve visualisation of both outflow tracts. As will emerge (and as it emerged during the trial) the illustration of the technique in Figure 3 in the guideline (which is reproduced below) does have to be viewed in the light of the sub-script to the illustration because the illustration itself could give the impression that the whole scanning motion was simply in one plane. That is not entirely accurate. Ms Edwards described the illustration as a "simplistic diagram of what we do". Figure 3 is as follows:
- The subscript to the above illustration says this:
"Fetal heart scanning technique. The four-chamber view of the heart is obtained from an axial scanning plane across the fetal thorax. Corresponding views of the left (LVOT) and right (RVOT) ventricular outflow tracts are found by angling the transducer toward the fetal head. Reproduced with permission from: Lee W. American Institute of Ultrasound in Medicine. Performance of the basic fetal cardiac ultrasound examination. J Ultrasound Med 1998; 17: 601607."
- The important matter to note from the subscript is that the transducer has to be "angled toward the fetal head" in order to visualise the LVOT and the RVOT. Although it is difficult for me to make this conclusion with complete conviction given the two-dimensional nature of the diagram, it is possible that the arrow in the second part of the illustration suggests a turning movement towards the fetal head. I will return to this issue later (see paragraphs 40-46 below).
- Although this guideline was introduced in 2005, the desirability of identifying the outflow tracts in addition to the "four-chamber view" had been canvassed in the literature for at least 20 years prior thereto: see 'The Aortic and Pulmonary Outflow Tract Screening Examination in the Human Fetus' by DeVore (Journal of Ultrasound Medicine, 11-345-348, 1992).
- The relevant NHS Guidance at the material time had been given in 'NHS Fetal Anomaly Screening Programme 18+0 to 20+6 Weeks Fetal Anomaly Scan, National Standards and Guidance for England' (the 'FASP Guidance'). It was published in January 2010, but its impact could not be instantaneous and a period during which NHS Trusts throughout the country implemented the guidance was contemplated. It should be noted that Dr Chudleigh and Professor Soothill were members of the National Ultrasound Screening Standards Core Reference Group, which was the body responsible for producing the guidance, and indeed Professor Soothill chaired the group.
- In relation to the fetal heart, the guidance required a "Four-chamber view" to be obtained and a view of the "Outflow tracts". In Appendix 3 of the guidance (the Fetal Cardiac Protocol), the following appears:
"Fetal echocardiography involving the four-chamber view of the heart and the outflow tracts forms part of the 'ultrasound scan base menu'. As a minimum, four basic intracardiac views are required they are: laterality, the four-chamber view, the left ventricular outflow tract and the right ventricular outflow tract."
- The FASP Guidelines at that time did not require archiving of any ultrasound cardiac images although, as will appear, it had already been Mr Jayasinghe's practice to retain some still images in the mother's file and elsewhere. These were obtained by "freezing" the moving image and saving it.
- Mr Jayasinghe said (and it was not disputed) that the FASP offered to provide further training on cardiac scanning in hospitals and that it happened in the Princess Royal University Hospital at the end of 2011 and was completed in early 2012. It does follow that he had not received any further training based upon the FASP guidelines at the time that XXX's mother was scanned. In his response in July 2012 to the complaint made by her about a year later, he said this:
"Over a year ago we only had limited experience in checking for cardiac abnormalities (outflow tracts etc) during an anomaly scan."
- Notwithstanding the terms of the 2010 FASP Guidelines, the hospital's own Ante-Natal Scanning Guideline issued in September 2006 (and still extant at the time of the scan in this case) required, as part of the "Anomaly scan", a scan of the thorax "including 4-chamber view of fetal heart (photograph) and great vessels." Mr Jayasinghe confirmed that this meant that he was required to identify and retain a photograph of the four-chamber view and that he should identify the LVOT and the RVOT, but that there was no obligation to record a photograph of either of those vessels unless there was thought to be an anomaly.
- I will return to what Mr Jayasinghe did (or believes that he did) on the material occasion (see paragraphs 47-58 below), but it has not been disputed that as at July 2011 the requirements of reasonable ultrasound scanning practice in England demanded an ability on the part of the person undertaking the 20-week scan to identify a normal LVOT and RVOT as separate features in order for the scan to be reported as normal.
The required scanning technique in more detail
- I have referred to the technique illustrated in the ISUOG Guideline above (see paragraphs 25-30). Although "simplistic" (see paragraph 28 above), it does essentially illustrate what the majority of the experts on both sides in the case regard as the established, proper technique for identifying whether there was a separate LVOT and a separate RVOT. It was the technique used at the time.
- The technique has been described as "the sweep technique" (which is how it was described in a more recent revision of the ISUOG Guidelines). Reference to those up-dated Guidelines shows how the technique is described. In the descriptive text, reference is made to "Figure 4". There are two elements to Figure 4 which are produced below. In the first diagram there are 5 stages or aspects of the scanning view displayed and, moving from right to left on the diagram, the views are labelled 'four-chamber', 'LVOT', 'RVOT', '3V' (three-vessel) and '3VT' (three vessels and trachea). The final two views thus labelled can be ignored for the purposes of this case.
- The scanning technique is described in the sub-script to Figure 4 as follows:
"The four-chamber view is obtained through an axial scanning plane across the fetal chest. Cephalad tilting of the transducer from the four-chamber view towards the fetal head gives the outflow tract views sequentially: left ventricular outflow tract (LVOT), right ventricular outflow tract (RVOT), three-vessel (3V) and three vessels and trachea (3VT) views."
- The text itself says this:
"The LVOT and RVOT views can be obtained by sliding (or angling) the transducer towards the fetal head (sweep technique) (Figure 4), starting from a four-chamber view to obtain the normal cross-over of the aorta and main pulmonary artery at their origin
."
- The text does go on to describe an alternative technique in this way:
"Alternatively, a variation in the method for evaluating the outflow tracts in the fetus has also been described: the rotational technique
. From a four-chamber view of the heart, the transducer is first rotated towards the fetal right shoulder. This technique, more easily performed when the interventricular septum is perpendicular to the ultrasound beam, may require slightly more manual skills but optimizes visualization of the LVOT, especially the septoaortic continuity. It also allows visualization of the whole ascending aorta, as opposed to only its proximal part as with the sweep technique."
- I mention this alternative technique (which became known as the "rotational technique" during the trial) simply because, for a while during the evidence, there appeared to be a suggestion on behalf of the Defendant that it was this technique that Mr Jayasinghe used (see paragraphs 56-57 below). The suggestion was that its use (which would have been legitimate) may have led to a misidentification of the RVOT because it involved visualisation of the LVOT and the RVOT "at different time points and in different planes". Ultimately, it was common ground (or substantially common ground) that it was not the technique that he had described himself as using and, accordingly, the relevance of the alternative technique (which had been described in the paper referred to in paragraph 31 above) to the issues in the case disappeared. Mr Whitting, in due course, called it a "red herring".
- The text following the reference to this alternative technique does, however, continue thus:
"With both techniques, once the LVOT view is obtained, the transducer is angled cephalad[1] until the pulmonary artery is observed with a direction almost perpendicular to that of the aorta."
- That short passage suggests that whichever technique is involved, the movement of the transducer after the LVOT view has been obtained is a continuing movement until the pulmonary artery (which is the source of the RVOT) is seen. I will turn to the views of the experts shortly (see paragraphs 88-104 below), but my perception is that the sweeping movement described and required is effectively one movement or one sequence of scanning designed to demonstrate two separate outlet tracts, one being seen more or less immediately after the other: taking views as separate incidents from different angles, rather than scanning in one sequence, runs the risk of the sonographer being misled by seeing the same structure from two different viewpoints and believing that he or she has seen the LVOT and the RVOT. The logic behind adopting the technique I have endeavoured to describe seems to me to be inescapable and this may have a bearing on my evaluation of the expert evidence (see paragraphs 101-104 below). That said, I thought that at the end of the debates that took place during the trial, there was a substantial (though not unanimous) measure of agreement that the technique I have endeavoured to describe was the only technique that ensured that the sonographer would see an LVOT and an RVOT without the risk of one being mimicked by the other (see paragraphs 88-100 below).
- The technique is illustrated on an FASP training video that was drawn to my attention after much of the evidence had been given. Dr Frances Bu'Lock, the Consultant Fetal Cardiologist called for the Defendant, produced the video to the court and she and Dr Chudleigh commented on it. In fact, Dr Chudleigh is seen in the video demonstrating the technique required to obtain the RVOT view. It is, of course, difficult to reproduce accurately in descriptive form in this judgment precisely what the video shows, but it starts with demonstrating how the four-chamber view is obtained, very much along the lines of the diagrammatic representations shown in paragraphs 28 and 39 above. The section of the video describing how to obtain the LVOT view shows the transducer being turned around upon its vertical central axis from the position required to obtain the four-chamber view towards the fetal right shoulder and moved slightly upwards ("sliding up slightly to the LVOT", as Dr Chudleigh put it). From the LVOT view the transducer is angled towards the fetal head in a transverse section by pivoting it backwards on its central horizontal axis so that the ultrasound beam is in an upwards plane in the direction of the fetal head ("sliding up slightly and rotating to the RVOT", according to Dr Chudleigh). Each of these positions is illustrated in the screenshots reproduced in Appendix 3 to this judgment. This description and these images best illustrate the "angling" or "turning" required in carrying out the sweep technique, phraseology that caused some confusion in the earlier stages of the trial.
What happened when the scan was undertaken on 7 July 2011?
- Mr Jayasinghe conducted many scans at the material time - apparently, he conducted 1,230 foetal anomaly scans during 2010-2011. Not surprisingly, he has no independent recollection of the scan undertaken on 7 July 2011. When the first complaint was made in July 2012 (see paragraph 35 above), he was not able to remember anything about it. He has had to rely throughout upon what he says was his standard practice at the time and on the inferences that can be drawn from the images he did preserve.
- In his witness statement, he described the general arrangement, with XXX's mother lying supine with her abdomen exposed. He said that the timing on the ultrasound machine was probably incorrect with the consequence that the timings on the retained images were also incorrect. That is of no consequence in this case, but the sequence in which the images were recorded can be ascertained from the timings shown on those images.
- Identifying the lie of the baby was, of course, important so that the transducer could be directed appropriately. He noted at the time that the baby here was in a longitudinal lie with breech presentation (in other words, the head was up within the uterus). He described what he would have done by way of observation of organs other than the foetal heart. So far as the foetal heart is concerned, he said this:
"23. I would have looked at the foetal heart in detail. I would have looked at a cross section of the baby's chest, before finding the optimum view of the heart
. This is something that I would have done by moving the ultrasound probe around dynamically. I would have looked for a cross section of the baby's chest to look for four chambers of the heart. It appears that I have not been able to get an optimum image of the four chambers of the heart at this time due to the position of the baby. However, I have identified the left ventricle outflow tract of the heart clearly
.
24. Sometimes, it is necessary to ask a patient to turn to the side slightly to achieve the best view. I would have had to try different angles to get the correct view, and probe until I could see all of the appropriate landmarks clearly. If I am unable to see clearly enough, I would usually ask the patient to take a break from the scan, go for a short walk, and return about half an hour later. Depending on the positioning of the foetus, it can be difficult to see clearly. In this instance the baby was breech and, while I cannot say that this posed a difficulty necessarily, it may have been that the baby was lying in a difficult position.
25. Looking at the images and their timings, I believe that I may have asked [XXX's mother] to come back after a short while as there is a gap in the timings of the images. This suggests that I may not have seen enough to be satisfied on the first occasion, and required her to come back again for a second look. However, this is not unusual, and it would certainly have been my normal practice to ask her to return."
- He went on to describe how "later" he was able to obtain a four-chamber view of which he retained a photographic record. He said that he did not observe any breach of the ventricular septum which appeared intact.
- In relation to the outflow tracts he said as follows:
"30. I would have checked for the right and left ventricular outflow tracts after obtaining a four-chamber view. I was not required to archive any images of the foetal heart views in accordance with FASP 2010 standards. It can be difficult to obtain a clear image of this once the picture is frozen, when it is compared to dynamic real-time images. I would have angled the transducer toward the foetal head and directed it in different directions to demonstrate the outflow tracts
.
31. When the transducer was angled towards the baby's head to check the aorta, as the main artery arising from the left ventricle, the anterior wall of the aorta appeared to continue with the ventricular septum, which led me to believe that the ventricular septum was intact. The image of the left ventricular outflow tract also suggests that the ventricular septum was continuous and appeared normal. If there was a defect, I would have expected to have seen a gap; although, there is no gap or break in continuity on this image. For my observation, I did not observe an abnormality of the outflow tracts. In real-time, the outflow tract would have appeared normal on both the right and left, insofar as I can ascertain from [XXX's mother's] records."
- Having looked at the images he retained and the times at which the various images were recorded as having been taken, Mr Jayasinghe says that they demonstrate that he could not obtain a four-chamber view at his first attempt, although he was able to identify what he thought was the LVOT view. Since it was necessary to obtain a four-chamber view, he asked XXX's mother to go away for a while and return later during which time it was hoped that the baby would have moved into a more convenient position for the purposes of scanning. From the timings, it looks as if she went away for about 30 minutes and then returned. On this occasion Mr Jayasinghe did achieve (and retained an image of) a four-chamber view and he did achieve (and retained an image of) what he thought was the LVOT view about one minute later. It is accepted that the four-chamber view that Mr Jayasinghe recorded was normal and that it was reasonable to interpret the image he retained and labelled the LVOT view as the LVOT view.
- In his oral evidence he expanded on the description he had given in paragraphs 30 and 31 of his witness statement concerning the technique he would have used. Ms Gumbel QC protested that he was describing in considerably more detail what he had put in short form in the witness statement. However, since the net effect of what he said ultimately was that he attempted to use the sweep technique (which is what he had described shortly in his witness statement), no particular difficulty arose in consequence.
- He said that once he had achieved properly the four-chamber view he would have "angled the transducer towards the baby's head and slightly towards the right shoulder". He would look for the LVOT and the RVOT to "see whether they [looked] normal and from different directions". He explained that the aorta "goes in one direction and the pulmonary artery normally goes in a slightly different direction" so that "if they are in different positions, [he] would have seen and checked whether it looks normal". After obtaining the four-chamber view, he said the transducer is moved "in order to get the correct view" and that it was quite quick in practice when that is done. In cross-examination he said thus:
"You are doing the four chambers and then angle one way to demonstrate the left ventricular outflow tract and then slightly the other way to demonstrate the right ventricular outflow tract. That was the technique I was using at the time."
- He was asked roughly what time difference there would have been between visualising the LVOT and then moving the transducer and obtaining a good image of the RVOT? As I understood his answer, it was that it would only be about 30 seconds later because, before he moved to find the RVOT, he would have wanted to assess the ventricular septum "to see whether it is continuing with the aorta". That would take about 30 seconds.
- When he was asked (without the ISUOG Guidance being put directly to him) whether the technique he used was a sweep technique or a rotational technique he said it was
"
the rotational technique, I would say, because what I did was from the four-chamber view I would angle the transducer in different directions, so it is the rotational technique."
- This was the beginning of the issue about the use of the rotational technique which, in due course, disappeared from the case (see paragraph 43 above), but Ms Gumbel has drawn attention to the fact that this was the first occasion that there had ever been any suggestion that Mr Jayasinghe used what is termed the rotational technique. She is right: there was no reference to it in the Opening Note and nothing in any of the experts' reports or joint statements that raised it.
- It is to be noted that, when presented with the complaint in July 2012 (see paragraphs 35 and 47 above), in his response he did not specifically list the LVOT and the RVOT as "anatomical structures" that he checked nor did he refer to having seen the RVOT. He does mention that the "[ventricular] septum [appeared] to be continuous with the anterior wall of the Aorta, in the [left] ventricular outflow tract view." It is, of course, clear from the images he retained that he thought he had seen the LVOT so it follows that he must have adopted a technique that led him to record this. He did not retain an image of the RVOT view that he says he obtained, but it was not mandatory for him to do so.
- It was the view of the majority of the experts that what Mr Jayasinghe described as the technique he would have adopted was the sweep technique. If Mr Jayasinghe did perform the sweep technique properly, then it is common ground that there could be no criticism of what he did. However, the crucial question is whether he did carry it out "properly", in other words, whether his actual implementation of the sweep technique on this occasion was to a reasonable standard. If it was not and/or he simply failed to record and report an anomaly that he in fact saw, then a case in negligence would be established. This issue falls to be addressed against the background of two matters raised on behalf of the Defendant: (i) whether, as Mr Whitting has suggested, there is a "significant, flaw in the Claimants' case [because of the] common ground that a very significant percentage of fetal cardiac abnormalities are not detected on routine anomaly scan"; (ii) that there was something so significantly unusual about XXX's fetal cardiac anatomy that even a competently executed sweep technique would have missed the abnormality because of mimicking.
- I will deal with each of these issues before returning to the issue of whether it has been established that Mr Jayasinghe must have missed the anomaly through a defective technique on this occasion.
The statistics
- The material sought to be deployed on behalf of the Defendant was designed to demonstrate that, even with a competently executed scan, it is possible for an anomaly such as this to be missed.
- Mr Whitting's starting-point was that, whatever may be the precise figure (about which there was debate between the experts), it appeared to be agreed, in broad terms, that a significant proportion of such abnormalities are missed and that it cannot be that all of those abnormalities are missed because of negligence in the sonographer's technique. Indeed, his written closing submissions contained the assertion that "it is common ground that even in the most skilled and experienced hands, the anomaly scan will routinely fail to detect truncus." I do not consider that he is correct to say that this was common ground and, in any event, I do not consider that the evidence supported the proposition that a properly executed anomaly scan routinely fails to detect truncus arteriosus. Ms Gumbel acknowledged at the outset that not all cardiac abnormalities can be detected and that the failure to detect such an abnormality is by no means of itself evidence of negligence, but contended that this case is one where the abnormalities present should have been detected by the views required to be obtained.
- Returning to Mr Whitting's proposition, in the first place, it is necessary to recall that the purpose of the scan is not to "detect truncus arteriosus", but to see if there is concern that a separate LVOT and RVOT cannot be identified on the scan. If so, the mother needs to be referred for further investigation (see paragraph 21 above).
- Mr Whitting relies, as I understand it, on a passage in his cross-examination of Dr Chudleigh for the purpose of sustaining his contention. I should record it, noting that the questioning started by reference to her membership of the group referred to in paragraph 32 above:
"Q. Can you tell us -- you were on the committee what the actual detection rate was for serious cardiac abnormalities at that time?
A. There was very little routine data available from routine screening programmes, which was one of the problems. A lot of departments or a lot of groups would have used the data from the Bull study, which had a detection rate of around about 30 per cent, I think, or 35 per cent for cardiac abnormalities.
Q. When was that study published?
A. Off the top of my head, I think 1999.
Q. That was the most recent study you had available when you were setting a target of 50 per cent?
A. That was what we used because that was data that the group felt was representative of what was being undertaken in the UK at that time, although it did not include outflow tract abnormalities in all of the departments presented in the literature, so it was likely to be an under-representation of the detection rates ante-natally of cardiac abnormalities at that time. But the group felt that it was the best that we could use at that time from the UK data. The Norwegian data from Tegnander et al gave higher detection rates, but we wanted to use UK equivalent data.
Q. So the best data you had -- and I appreciate it was about ten years old at that stage -- in the UK was about 30 per cent and you set a target of 50 per cent in FASP?
A. That is correct.
Q. If 50 per cent -- and I appreciate that is simply a target rather than an actual outcome as at 2011 of serious cardiac abnormalities are not detected on an anomalies scan, the fact that one is missed in a particular case would not of itself mean the scan was incompetently performed, would it?
A. Correct.
Q. It is simply evidence of the limitations of ultrasound?
A. Depending upon what the abnormality was that was missed, correct, yes.
Q. In fairness to you, nowhere in your reports or in the joint statements do you suggest otherwise; you don't suggest that by definition it is negligent to miss a serious cardiac abnormality like truncus in this case?
A. Correct."
- I will return to that shortly, but it is, of course, important to recall that Dr Chudleigh's very clearly expressed opinion has always been that a properly implemented sweep technique in this case would have revealed that there was no separate LVOT and RVOT and that failing to observe or note this was negligent. She noted in her first report that there was nothing recorded (such as maternal obesity) to compromise the effectiveness of the scan.
- She was, in effect, asked whether "by definition" failing to identify truncus arteriosus (presumably, missing the indication of the condition by reference to the lack of a separate LVOT and RVOT) was negligent to which the answer was 'no'. This is no more than the concession made by Ms Gumbel at the outset to which I referred in paragraph 62 above. However, the more important issue is why there may be a failure to identify the warning sign thus identified. She gave maternal obesity as an example. Professor Soothill went into more detail in answer to a question from Mr Whitting about whether truncus arteriosus falls towards the more difficult end of the spectrum to detect on ultrasound scan. His reply was as follows:
"
the overriding answer to your question is, if you are not looking at outflow tracts, then you will not detect a large amount. If you are looking at the outflow tracts, there will still be some cases missed and there are all sorts of reasons for that; for example, twins, wrong gestational age, an overweight woman, polyhydramnios -- there are many possible reasons. I do agree that truncus arteriosus is not the easiest heart malformation to be seen, and that's because it is predominantly in the great vessels rather than mostly, if you like, within the ventricles, but it is not the hardest either. I mean, if you take coarctation of the aorta or anomalous pulmonary venous drainage, et cetera, they are much harder to detect than truncus arteriosus."
- Professor Soothill was thus simply saying that there may be a good number of reasons why a competently implemented scan at 20 weeks might miss the lack of separate LVOT and RVOT, but there is no suggestion that any of those reasons existed in this case. Professor Soothill's evidence, which struck me as objective, well-balanced and authoritative, subjected the material relied upon for the statistical analysis advanced to rather greater analysis than did Dr Chudleigh and his appraisal of the material, in the context of the arguments advanced by Ms Gumbel, have led me to the view that this issue has little relevance in this case.
- In short, there are, as it seems to me, a number of difficulties with the material relied upon to support any worthwhile statistical analysis. If one is looking for the statistical likelihood in July 2011 of non-negligently "missing" the kind of anomaly involved in this case, one would need a sufficiently large cohort of babies who demonstrably had the specific anomaly and in respect of whom (i) the sweep technique was adopted at the 20-week stage (or thereabouts) and (ii) which was carried out correctly, in order to have a statistically valid appraisal of the situation. If it could be shown that a statistically relevant proportion of the cohort were "missed" notwithstanding a competently executed scan of which the primary purpose was to identify an LVOT and RVOT, then the issue advanced by Mr Whitting on behalf of the Defendant may have some relevance. However, I do not consider that the evidence goes anywhere near demonstrating such a proposition.
- So far as the UK is concerned, it was only after the promulgation of the FASP guidance that it became effectively mandatory for sonographers undertaking the 20-week scan to look positively for the LVOT and RVOT, but (as indicated above: see paragraphs 32-33 above) the implementation of the guidance was not (and could not have been) instantaneous. Given the rarity of the anomaly, it would be surprising in the extreme if any worthwhile cohort could be identified in the period after the guidance was promulgated, but before July 2011. Indeed, no such material existed. On a somewhat more anecdotal level, Dr Bu'Lock and Dr Tsai-Goodman, with many years collective experience, had only had experience of a very limited number of "missed" anomalies of this nature between them. But, in any event, it would require clear evidence that a technique that could effectively identify the LVOT and the RVOT as separate vessels had been competently undertaken. Whilst, as Professor Soothill said in his evidence, some hospitals have been carrying out what he described as a "great vessel examination" prior to the promulgation of the guidance, the process was one of evolution and drawing conclusions from data from this period would be inconclusive. As I understood him, Mr Howe agreed with this reservation about the statistical material.
- As I have said, unless the material upon which any statistical conclusions are drawn are focused on a scanning technique that involves positively identifying the LVOT and the RVOT, there is little, if anything, of relevance to be derived from such statistics. Ms Gumbel is right to submit that statistics based upon the failure to detect "cardiac abnormalities" in general terms do not assist - and that is the scenario that lies behind much of the material relied upon in the various series reported which includes the paper by Boyd and others upon which some reliance was placed on behalf of the Claimants. It was entitled 'The evolution of prenatal screening and diagnosis and its impact on an unselected population over an 18-year period' published in the British Journal of Obstetrics and Gynaecology in June 2012. By reference to the period 2000-2008, the study showed a prenatal detection and termination of pregnancy for fetal anomaly rate in the local Oxfordshire population of 54% for "severe fetal anomalies". These are defined as including single ventricle, tricuspid atresia, Ebstein's anomaly, hypoplastic left heart, hypoplastic right heart, common arterial truncus, transposition of great vessels, atrioventricularseptal defects, tetralogy of Fallot, pulmonary valve atresia, aortic valve atresia/stenosis, coarctation of aorta and total anomalous pulmonary venous return." This was obviously not directed solely to CAT and the period involved was before the FASP guidance. The argument advanced on the Claimants' behalf was that an adjustment upwards from the 54% figure would be appropriate in the light of the need to include outflow tract views after 2008. This seems to me to be altogether too speculative to reach any sustainable conclusion. I recognise that Professor Soothill (and indeed Dr Chudleigh) gave some credence to this paper for this purpose, but it is, in my judgment, no more persuasive on the precise issue (namely, the rate at which the non-existence of an LVOT and/or an RVOT is missed on a properly conducted ultrasound scan) than any other series.
- Mr Howe had drawn on a paper by Pinto and others entitled 'Barriers to prenatal detection of congenital heart disease: a population-based study', which was a retrospective cohort study of cases with congenital heart disease (excluding minor defects) identified between 1997 and 2007 across the State of Utah in the USA. The result was that congenital heart disease was detected prenatally in only 39% of 1474 cases, with no improvement in detection rate over the 10-year period.
- Professor Soothill pointed out that the article indicated that 77% of the mothers had an ultrasound scan between 16 and 24 weeks gestation, which meant that 23% did not have such a scan at a time when the abnormality could reasonably have been looked for. He also said that the reasons why the detection rate was low was that the cohort would not have included women who declined screening or were too late to undergo it. He also said that it was not clear to what extent attempts were made to view the outflow tracks. He did not feel that the paper gave any help to the issue of detection rates of the UK. I have to say that those seem to be compelling points to which Mr Howe did not have a substantive answer and, in the end, I think that Mr Howe largely accepted this.
- Mr Howe also produced the Caris Review 2017 (i.e. the review produced by the Congenital Anomaly Register & Information Service for Wales) which showed that the detection rate for truncus arteriosus (based on the period from 2012-2016 because of the small numbers) was 44.4%. Professor Soothill said in the joint statement with Mr Howe that this sequence of cases had not been published in a form suitable to make an informed assessment because of the small numbers (which had not been stated) involved. It was not, he said, a peer-reviewed paper which gave details of the methodology, for example. He noted that it reports 66 cases of truncus arteriosus in the years 1998-2016, but the "denominator of [such] cases being reported for the detection rate is not stated and information about issues such as women not having a 20-week anomaly scan (because of late pregnancy booking, decline of screening etc.) is not given."
- Mr Howe said in the joint statement that the detection rate "demonstrates the inherent difficulties screening sonographers have at identifying this particular cardiac anomaly and the low sensitivity of UK practice at detecting it." In answer to the Defendant's Agenda for any revised opinion, he referred to this paper and said that "[it] is clear, therefore, that reasonable and competent screening sonographers undertaking routine anomaly scans fail to recognise this anomaly in a high proportion of cases, demonstrating the inherent difficulty of making this diagnosis."
- I am afraid that I consider that these observations significantly over-state what can be drawn from this paper which, in my view, adds little to the debate about the statistics or indeed about the efficacy of the scanning technique.
- Mr Howe also referred to some material derived from the Wessex area where he practises which suggested that the detection rate for truncus was 45%. It emerged that that was based on 20 cases between 1994 and 2011 (of which there were 9 true cases of truncus arteriosus). That, of course, was prior to the FASP guidance and, whilst he suggested that some hospitals in the area did look for the outflow tracts before the FASP guidance was given, he conceded that for at least 8 years of this period the hospitals did not routinely check for the outflow tracts and he accepted that until the FASP Guidance became available the sonographers would not have had the training and diagrams that became available thereafter. The number of truncus cases included cases of pulmonary atresia VSD (the detection rate for which was 24%) which Mr Howe said was a Type 4 truncus.
- I regret to say that I did not find this evidence very persuasive and, along with the other material Mr Howe relied upon to suggest a low detection rate for truncus arteriosus, I gained the impression that he was looking for support from a number of sources that, on a fair and objective analysis, did not truly support the contention he was advancing.
- Professor Soothill said that if sonographers are examining the heart correctly, they should be able to identify the fact that only one vessel is leaving the heart. This simple proposition, to which Dr Chudleigh and Dr Tsai-Goodman also subscribed, neutralises any impact that the very inconclusive statistics may have upon the outcome of the case. Since, as Ms Gumbel submits, the detection rates cannot be accurately ascertained for this condition under a regime that requires the LVOT and the RVOT to be checked for normality, there is nothing of value in the material to inform the issue of whether, on this occasion, Mr Jayasinghe negligently failed to notice sufficient abnormality to refer XXX's mother for further investigations.
XXX's unusual fetal cardiac anatomy
- The trial was originally due to be heard in January 2017, but the date had to be vacated at the last minute.
- Prior to the originally scheduled date for the trial it had been accepted by Ms Edwards that "a normal RVOT view could not have been obtained" and she went on to say that "the single vessel present was spanning the right ventricle and therefore from some angles may have looked like the RVOT but would not have coursed in the normal direction
towards the fetal spine." In its Notice of Application dated 27 September 2017 seeking the court's permission to rely on the evidence to which I will refer below, the Defendant accepted that this meant that it was agreed by the experts at that stage "that a reasonable and responsible sonographer would have been expected to have identified" the fact that the apparent RVOT was not going in the right direction.
- Furthermore, Dr Tsai-Goodman and Dr Bu'Lock had also agreed as follows:
"Mr Jayasinghe could have mistaken the one and only one outflow tract as two different outflow tracts. However, the orientation of the outflow tracts in relation to the 'assumed normal heart' could not have been normal and he should have questioned what he saw or referred if in doubt."
- At that stage, therefore, the case on breach of duty was all but established. However, based on the advice of Dr Bu'Lock, the Defendant commissioned a 3D reconstruction of XXX's heart preoperatively based upon any pre-operative imaging. This was carried out, based on the postnatal cardiac MRI scans, by Dr Saravnan Durairaj, a Consulant Paediatric Neurologist, based at the East Midlands Congenital Heart Disease Centre in Leicester. He is a professional colleague of Dr Bu'Lock. In a witness statement dated 18 October 2017 he described the technical processes adopted to produce the 3D images. The Claimants instructed Professor Tal Geva, a Paediatric Cardiologist at the Boston Children's Hospital in the USA, to review the reconstruction. He did so and recreated a similar 3D model from the images supplied to him. He was of the view that the 3D reconstruction was not relevant to the case and did not mitigate the "failure to diagnose a single exit from the heart". I did not hear directly from him and I will make my assessment of the value of the evidence on the basis of the witnesses I heard.
- This is yet another area in this case where it is very difficult to convey in written form the anatomical features that have figured in the new debate since the 3D model has been prepared. I received a detailed account from Dr Bu'Lock about what the model demonstrates and how XXX's cardiac anatomy was unusual. However, I think I can do justice to the debate with a short description of what Dr Bu'Lock says has been revealed about the cardiac anatomy and then indicate the views of the experts on the relevance of this information.
- In her Supplemental Report she described the normal heart and its development during the embryonic stage from a "primitive heart tube", in which the blood enters at the lower end of the tube called the 'truncus arteriosus', which itself then separates into its pulmonary and aortic components. She then described the congenital heart malformations known as "conotruncal malformations" where there is a "variable degree of failure of the normal separation of the left and right sides of the ventricular outflow tracts and the great arteries". She then went on to describe the known "variants" of truncus arteriosus. She says that it is "difficult to be precise about the relative incidence of each of the different patterns of separation of the aorta and pulmonary arteries but the majority are forms
where either there is a variable length of 'main' pulmonary artery of variable diameter giving rise to the branch pulmonary arteries and/or the branch pulmonary arteries arise from the posterior aspect of the trunk." She asserted that "the most usual type of truncus arteriosus would give the ultrasound of either very early splitting (bifurcation) of a single outflow great vessel or absence of any anterior structures and it is indeed less likely that this could be mistaken for normal on prenatal scanning." She says that XXX's cardiac anatomy was different:
"However, for [XXX], the variant noted postnatally, and described in detail at surgery
is completely different and extremely rare. Effectively the vessel above the truncal valve is both the main pulmonary artery and the aorta, as in one plane it gives rise to the right and left pulmonary arteries, and it continues in a different plane as[2] the aorta ...."
- It might be helpful to record how Dr Tsai-Goodman described the configuration in XXX's cardiac anatomy which she described in her oral evidence as "rather unusual". It was as follows:
"
the right and left pulmonary arteries both arise from the left-hand side with the right pulmonary artery curling round to the posterior aspect of the aorta."
- Dr Bu'Lock's conclusion was:
"In conclusion it is therefore clear that it is the very specific nature of [XXX's] rare congenital heart defect that provides a clear explanation as to why it would have been possible to obtain sonographic images in separate planes at the fetal anomaly screening scan which would have closely mimicked normal left and right ventricular outflows. Hence there is indeed a reason why a properly conducted scan by an experienced sonographer could generate the impression of normality."
- In her Supplementary Report, Dr Tsai-Goodman largely agreed with the descriptions given, but she disagreed specifically with the second sentence of the conclusion. She said this:
"I agree that the type of [XXX's] CAT is rare and unusual and that 'still' images often do not represent the true anatomy of the heart which is moving. The 'tube' just above the truncal valve is known as the truncus and would have separated into the pulmonary artery and the aorta in normal embryological 'life'. However, in CAT, the 'truncus' arising from both ventricles is neither the aorta nor the pulmonary artery. In [XXX's] CAT the first branch arising from the truncus is the right pulmonary artery and separately, the left pulmonary artery arises just above the right. The branch pulmonary arteries are not in the same plane
and therefore are not 'bifurcating' (i.e. one vessel dividing into two vessels in the same plane with the branches being connected) as in a normal heart. The trunk continues as the aorta into the aortic arch which is in a different plane to the pulmonary arteries but this feature occurs all types of CAT."
- She went on to explain why, in her view, the results of the 3D modelling made no difference to the case in the following way:
"
if the sonographer had followed the standard FASP axial planes, 'normal' looking right and left ventricular outflow tracts could not have been obtained. Non-standard views should not be used by a screening sonographer. If they are used, they run the risk of missing abnormal cardiac anatomy as I believe occurred in [XXX's] case.
I therefore disagree with Dr Bu'lock's conclusion that it is [XXX's] rare form of CAT that 'provided clear explanation as to why it would have been possible to obtain sonographic images in separate planes at the fetal anomaly screening scan that would have closely mimicked normal left and right ventricular outflow tracts.'
It continues to be my view that, on the assumption that, as the sonographer maintains, he was aware of the different orientation of the LVOT and RVOT, he could not have seen two differently orientated and distinctly separate outflow tracts nor two separate vessels in the normal views although he could have interpreted different views as such.
However, the only way of obtaining 'mimicking' views would have been by applying 'oblique' views/planes. Generally, those planes are used by specialists such as a fetal cardiologist who would understand the pitfalls of applying those views whilst scanning and who would have been trained in sequential analysis of the heart. Interpreting those 'oblique' planes/views is, in my understanding, outside the expertise of a screening sonographer. In any event it would be contrary to FASP guidance, the standard to which the sonographer was working."
- The true and material difference between Dr Tsai-Goodman and Dr Bu'Lock following the availability of the 3D model can be discerned from the following answers to various questions posed at their second joint discussion:
"It is agreed that it is impossible to genuinely see two great vessels as there is only one. It is however possible to mistake one single vessel as two separate vessels in this fetus as the trunk gives rise to two separate branch pulmonary arteries. The presence of the 'two vessels' could however only be inferred from interrogating the fetal heart from oblique angles and at different times. WE AGREE." (Emphasis added.)
"Mr Jayasinghe could not have obtained a truly normal RVOT view. However as previously highlighted, due to the nature of [XXX's] heart condition, a structure mimicking the RVOT could be mistaken for it. This could only have been obtained by imaging different parts of the fetal [heart] at different angles or approaches and at different times. WE AGREE." (Emphasis added.)
- This position was reflected in other answers. For example:
"In order for Mr Jayasinghe to interpret the single vessel arising from two different ventricles as 2 separate vessels he would have had to have taken images from different angles, orientations and at different times of scanning. It is impossible to have obtained those images in a single sweep starting from the horizontal /axial four chamber view and sweeping towards the fetal head." (Emphasis in bold is mine.)
- That answer indicates their agreement and, incidentally, reflects the view of Dr Chudleigh and Ms Edwards who said this:
"Mr Jayasinghe would not have been able to obtain the normal LVOT and RVOT views "simultaneously" at the same time point during the examination."
- Mr Howe did express a different view to which I will refer in a little more detail below (see paragraphs 101-104 below). For reasons I there express, I could not follow why he took that view, but at all events it was out of kilter with the views to which I have referred and it lacked what, to me, appeared to be the logic behind the technique acknowledged by the others to be appropriate.
- Reverting to the views of Dr Tsai-Goodman and Dr Bu'Lock, the following answers to the questions posed indicate where those views diverge:
Dr Tsai-Goodman
"In [XXX's] heart the trunk was overriding both ventricles and there was the same outflow tract for both ventricles and therefore by definition there cannot be a normal RVOT nor a normal LVOT. The 'normal RVOT' being slightly superior and at a different level to the 'normal LVOT', is also orientated in a different direction to the normal LVOT. The difference in space and in direction of two normal outflow tracts could not have been seen by Mr Jayasinghe as only one outflow tract was present. It is difficult to comprehend how the mimicking structure would have been seen by angling the transducer from the cross-sectional four chamber view towards the fetal head and directing it in different directions. The structures that mimicked the RVOT could only have been obtained by imaging that part of the heart in isolation rather than as part of a complete assessment of the heart." (The underlining is as in the original, the bold text is my emphasis.)
Dr Bu'Lock
"However as described in [earlier] answers
, a single sweep is neither required nor is it always feasible. The common trunk arose from both ventricles and could therefore presumably have been viewed as arising from the right ventricle (in a similar way to the LVOT view which was recorded). Although there is a single direction of the trunk, in [XXX's] case it is clear from the 3D
reconstructions that a mimicking view could indeed have the appearance that the Right Ventricular connection to the branch pulmonary arteries is in a different direction than the Left ventricular connection, due to the relative differences in spatial relationship of the two chambers to the proximal part of the Trunk. I agree that this structure would have needed to be viewed from a different angle. However, imaging the organs from a different angle is not a breach of practice." (The bold text is my emphasis).
- This difference of position was repeated in other answers posed in the Agendas of each party.
- When Dr Tsai-Goodman was challenged by Mr Whitting about the way she had expressed herself she said this:
"What I meant
is, if you did an axial sweep to the head, you would have not missed the fact that this baby had truncus arteriosus. If you individually just scanned the four chambers, then not look at the heart, come from another view and happen to see a structure that may mimic the right ventricle outflow tract and then move the probe and come from a different way and looked at the heart and happened to see something that looked like a LVOT, yes, you could. But by doing a sweep all together you would not have missed a truncus arteriosus." (My emphasis.)
- What I understood Dr Bu'Lock to be saying was that a "single sweep" is not always feasible and is not "required" (presumably by the FASP Guidance) and that viewing the organs from different angles is "not a breach of practice" and thus not negligent. Dr Tsai-Goodman says that a "complete assessment of the heart" can only be carried out properly and effectively by adopting the sweep technique. I have already observed (see paragraph 45) and will repeat below (see paragraphs 102-104) that the logic behind this seems inescapable on the evidence that has emerged in this case. It is correct that the FASP Guidance does not state explicitly that the technique should be adopted, as Dr Tsai-Goodman accepted. However, both Dr Tsai-Goodman and Dr Chudleigh taught this technique and it appears to be illustrated in the training video to which I have referred. I did not understand Ms Edwards to have a different view of how the technique is carried out. The technique was not a new technique as at the time of the FASP guidance. Those who were expected to identify an LVOT and an RVOT prior to the implementation of the guidance would need to have known about and adopt this technique.
- In his written Closing Submissions, Mr Whitting said that the "evidence of all of the experts was quite clear" namely, that "the technique described by Mr. Jayasinghe (a) involved, by definition, the outflow tracts being visualised at different angles or planes and at different times and (b) was entirely acceptable." I have re-read several times the passages in the transcript to which he referred in which, he asserted, concessions to that effect had been made by Dr Chudleigh and Dr Tsai-Goodman (and, to the extent, that he made any contribution to the debate on technique, by Professor Soothill) because that had not been the impression I had gained when listening to the evidence. Having done so, I am quite confident that my perception of what each of them said when giving evidence was correct. I will refer simply to one such passage in the cross-examination of Dr Chudleigh, because she is the experienced sonographer who demonstrated the relevant technique in the FASP demonstration (see paragraph 46 above and Appendix 3):
"Q. But I think the point that you are making because Mr Jayasinghe says, "Yes, I did see two separate vessels", but the point you are making is that you would have to see them at the same time so that you could differentiate the two?
A. No, you don't need to see them at the same time; you see them in different slices, one below the other. So you don't see the two vessels at exactly the same time in the same ultrasound section. You should see the two vessels within the same timeframe
. So if you were doing your correct examination of the heart from your four chambers sliding up to your LVOT, then sliding up to your RVOT, with a little bit of rotation
that is what I consider as seeing them separately in the same timeframe." (My emphasis.)
- Seeing the LVOT and the RVOT "separately in the same timeframe" grapples rather well, if I may say so, with the difficult descriptive exercise involved in trying to paint the picture of the technique involved. It is that technique to which I have been referring above.
- Mr Whitting made the following submission, after referring to those passages in the transcript where, he said, concessions about the technique had been made:
"The ineluctable effect of those concessions (and the conclusion which the Defendant urges the Court to draw), in the light of the consensus reached in the joint statements, is that, while adopting an entirely appropriate sonographic technique, Mr. Jayasinghe visualised, and was understandably reassured by, a mimicking structure of the RVOT (as he had been in respect of the LVOT). The reluctance of the Claimants' experts to accept that to be the case did them little credit and their respective attempts to avoid the logic of the evidence were wholly unconvincing."
- As I have indicated, I am quite unable to accept the contention that concessions of the nature suggested were made and, accordingly, that the position adopted by all three experts "did them little credit". I must assume that Mr Whitting is suggesting that they have trimmed their evidence to fit the case that was being advanced at the trial. If that is so, I do not accept it. Once the language used had been penetrated so that a clear understanding of their view could be obtained, the logic behind what they were saying became apparent. The countervailing logic is that a technique that involved the visualisation of "the outflow tracts
at different angles or planes and at different times" ran the serious risk that one vessel could be mistaken for the two separate vessels. All of them had accepted, once the results of the 3D reconstruction had been drawn to their attention, that the potential for mimicking existed in XXX's case. Their position, subject only to the difficulties of articulating it on paper, was consistent throughout: even with the potential for mimicking, a properly executed sweep technique should have revealed the lack of separate outflow tracts.
- Dr Bu'Lock's position was that a technique that did involve the identification of "the outflow tracts
at different angles or planes and at different times" was acceptable. The position taken by Mr Howe was different and did conflict with the position taken by all the other experts with appropriate expertise and experience. His view was that a properly executed sweep technique applied to XXX's fetal cardiac anatomy would have revealed views both of an LVOT and an RVOT. This was said on a number of occasions, but I will simply highlight a question designed for confirmation from Ms Gumbel and Mr Howe's answer:
"Q. If Mr Jayasinghe had conducted a sweep starting at the four-chamber and gone up in either slices or a sweep, as is described in the two diagrams, he could have seen what would have appeared a normal LVOT and a normal RVOT in the same sweep procedure. Is that your evidence?
A. Yes, it is."
- The two diagrams referred to in the question are the diagrams that appear in paragraph 28 above.
- This does conflict with the views of Dr Bu'Lock and Dr Tsai-Goodman as revealed in their answer referred to at paragraph 90 above.
- I am troubled that Mr Howe's answers may have opened up a division between him and the other experts that may be more apparent than real, but he did seem to accept that there was a divergence of view when asked specifically about it by Ms Gumbel. He is plainly an expert with relevant experience to offer the court, but since his view on this does seem out of step with the other expert evidence, I do not really have any option but to express my preference on this occasion for the views expressed by the others which, to my mind, have a more compelling logic to them.
Finding as to what happened on 7 July 2011
- Why did Mr Jayasinghe miss the fact that there were not two separate outflow tracts? Subject to the view of Mr Howe (which I have not felt able to prefer), it is broadly common ground that if he did execute the sweep technique as he described it, he should have identified the lack of two vessels. I think it highly unlikely that he would not have made a note (in the physical sense) that he did not see two outflow tracts if he did not see them. In other words, I think it highly unlikely that this was an instance of inadequate note-keeping. I consider it much more likely that he saw what he thought was an LVOT and a RVOT and was, accordingly, satisfied that everything was normal so far as these matters were concerned.
- Was this because of the unusual nature of XXX's cardiac anatomy and thus because of the consequent mimicking? I do not think so. If he carried out a proper sweep technique, I accept the views of Dr Chudleigh and Dr Tsai-Goodman, in particular, that he would not have missed the lack of two separate outlet tracts notwithstanding the unusual configuration in this particular case.
- There are, therefore, two potential explanations: either that his technique on this occasion was simply inadequate for the task he was undertaking and he inadvertently found the two views, one of which, properly speaking, was a mimicked view; or that he was not using the sweep technique at all and was using a technique that involved looking at the relevant anatomical features at different times and in different planes. Given that the images he retained of the four-chamber view and the LVOT (as he thought it was) were taken within a short period of each other (see paragraph 55 above), this suggests that he certainly embarked on what was the standard sweep technique and not on some alternative technique. It is now impossible to say precisely how he continued with the sweep technique, but, subject to the matters to which I will refer in paragraph 108 below, the likelihood is that he inadvertently moved the transducer in a way that, whilst he intended to continue with the sweep technique, in fact he did not do so and, in consequence, obtained a view from a different plane such that he saw a mimicked, apparently separate, outflow tract.
- The background factors to be considered in trying to reach a conclusion about what happened are twofold, in my view. First, Mr Jayasinghe was undoubtedly a very experienced sonographer and, I have little doubt, very conscientious in his job. However, there is no evidence about how often, if at all, he had previously noted a lack of separate outflow tracts even though he had been routinely looking for them since 2006. CAT is a rare complication and it is possible that he had never in fact been confronted with the issue previously. As I have said, there is no evidence, one way or the other, about that, but positive evidence that he had previously noted such an abnormality might have added to the more reassuring scenario that he knew how to find the anomaly if he needed to. Second, whilst he was undoubtedly a very experienced sonographer, he had not received the training that FASP considered advisable by the time he carried out the scan in July 2011 (see paragraph 35 above). That was not, of course, his personal fault, but it does raise the question of whether he was as au fait with the proper implementation of the sweep technique by then as, according to the standards by which his actions must fall to be judged (see paragraphs 11 and 37), he should have been.
- I consider that both factors may have played some part in his missing the signs of the abnormality on this occasion and being misled by what he saw. The most likely failure in the technique adopted on the evidence I have heard is that he inadvertently permitted the transducer to move from a continuous sweeping movement in the manner described and required above into a different plane such that the image of what he thought was a different outflow tract from the outflow tract seen previously was in fact the same one seen from a different angle. It is a relatively straightforward conclusion to reach on the evidence and, whilst the legitimate desire of the Defendant to defend a claim that appears defensible is understandable, I do not consider that either of the possible explanations put forward for missing the abnormality answers that conclusion on the basis of the evidence I have heard.
- Regrettably, this does mean that the conclusion must be that the scan was not carried out to the required standards of the time.
Would XXX's mother have had a termination of pregnancy?
- This kind of issue is always difficult and sensitive and Mr Whitting approached it with sensitivity which I am sure was appreciated by XXX's parents. It is also difficult for the parents in a situation such as this to put out of their minds the events that have occurred and the knowledge they have acquired since the birth of the child in question. Having seen and heard from them both briefly, I am quite certain that they would have given what they would have been told about the likely or possible consequences of the 22q11.2 deletion syndrome with considerable care.
- XXX's mother said this in her witness statement:
"If [XXX's father] and I had been told about [XXX's] heart defect and 22q11.2 deletion syndrome we would not have continued with the pregnancy. If we had been told that he would need multiple complex heart surgeries and possibly have developmental delay as well as possibly a lot of other complex medical problems that can be associated with 22q11.2 deletion, we would have made the decision to put our daughter
first and terminate the pregnancy. We would have found the uncertainty around this condition unbearable."
- At the time of her pregnancy with XXX, her daughter was nearly 4 years of age and she wanted to be on maternity leave when her daughter started school. She agreed that the timing of XXX's birth was broadly planned, but said that if she and her husband had been told that XXX had a complex heart defect, which would have required "multiple surgeries" as well as the other possible consequences, that would have been enough for them. When asked about certain reassuring things that might have been put to them by the doctors giving them advice at the time (such as that the vast majority of babies born with this syndrome have successful corrections) she said this:
"I think I would have probably Googled things, I would have looked at Max Appeal, which lists in excess of 180 possible associations with this, and I think the not knowing and the possibility of psychosis and mental health issues and learning delays and a complex heart defect that needed immediate life-saving surgery and multiple surgeries throughout his life and the fact that this would be a condition
that would need ongoing care throughout his life - he would not just be fixed after the surgery - that would be enough for us to want a termination."
- When pressed further she said this:
"I still think that multiple heart surgeries requiring care throughout his entire life, the uncertainty regarding -- and it is uncertainty because you don't know --
psychiatric issues, bipolar, schizophrenia, all of these things which could or could not appear later in life, plus learning difficulties, that would have been enough for us."
- Her husband confirmed that they would both have discussed the issues had they been confronted with them at the time and ultimately the decision would have been that of his wife though he would certainly have had an input.
- As with all factual issues, this must be determined on the balance of probabilities. It would inevitably have been a difficult and unenviable decision, but I thought both parents were very level-headed, rational people who would have reached an objective and logical decision. Having regard to the various uncertainties and bearing in mind the interests of their daughter also, I accept, on the balance of probabilities, that they would have opted for a termination.
Conclusion
- The net effect of this judgment is that the Claimants have established the case advanced on the basis of breach of duty and causation and judgment must be entered for damages to be assessed.
APPENDIX 1
List of Experts
Claimant's experts
Dr Patricia Chudleigh, BSc, PGCHE, PhD, DMU
Dr Chudleigh has 30 years clinical experience in obstetric ultrasound and is currently employed by Cambridge University Hospitals NHS Foundation Trust as a specialist sonographer for Education and Training for routine obstetric ultrasound services at the Rosie Hospital, a maternity hospital. She has an impressive CV and played a role in the formulation of the FASP guidance and training. She is not medically qualified - her PhD was obtained in relation to ultrasound screening matters.
Dr Beverly Tsai-Goodman, BM, MD, FRCP
Dr Tsai-Goodman is a Consultant Paediatric and Fetal Cardiologist with a specialist interest in congenital heart disease in children and the unborn child. She is currently based at the Royal Brompton Hospital in London, but prior to that appointment she had been a Consultant Paediatric and Fetal Cardiologist (with a sub-speciality interest in non-invasive imaging) at the Bristol Royal Hospital for Sick Children since 2004. She also has an impressive CV and has also been an expert adviser to one of the FASP working groups.
Professor Peter Soothill, MBBS, BSc, MD, FRCOG
Professor (now Emeritus) Soothill was, until his retirement from clinical practice is 2015, a Consultant in Fetal Medicine with special interest in ultrasound screening, diagnostic ultrasound and other aspects of fetal development and therapy. He became a Consultant in 1992 and held positions, first, at UCL Hospitals and Great Ormond Street Hospital and then, second, from 1995 until his retirement at University Hospitals Bristol at St. Michael's Hospital. For about 7 years until January 2012 he had been Chairman of the Steering Committee of the FASP programme.
Defendant's experts
Ms Hazel Edwards MSc, PGCE (TLHE), DCR(R)
Ms Edwards is a sonographer who has experience of fetal anomaly scans in a general hospital setting since 1998. She is currently the senior sonographer with the East and North Hertfordshire NHS Trust. Prior to that she had been a consultant sonographer with the Norfolk and Norwich University Hospital. In 2012, she was invited to join the FASP working party to review the then cardiac protocol.
Dr Frances Bu'Lock, BM, BCHIR, MD, FRCP
Dr Bu'Lock is a Consultant and Associate Professor in Congenital and Paediatric Cardiology at the East Midlands Congenital Heart Centre in Leicester. She has been actively involved in fetal cardiology for over 20 years. She has an impressive CV and has worked in a number of units around the country. She has played a role in the "roll out" of the FASP programme in the East Midlands.
Mr David Howe, DM, FRCOG, FRCS(Ed)
Mr Howe is a Consultant in FetoMaternal medicine in the Wessex Fetal Medicine Unit at the Princess Anne Hospital in Southampton. His clinical practice is in obstetrics, managing complex pregnancies. His role includes the ante-natal diagnosis and management of fetal anomalies using ultrasound and other techniques. He has over 20 years' experience in this area.
APPENDIX 2
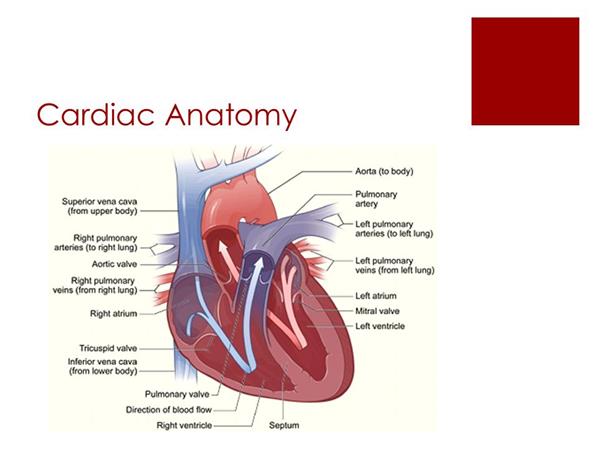
APPENDIX 3
The FASP training video
OBTAINING THE FOUR-CHAMBER VIEW

OBTAINING THE LVOT VIEW
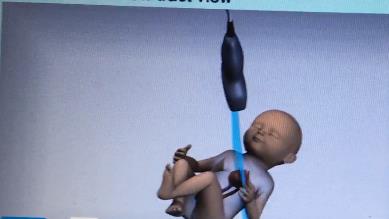
OBTAINING THE RVOT VIEW